 Supplied
Supplied
Alex Allan is a nutritionist and said more needs to be done for women who have polycystic ovary syndrome
When Alex Allan was diagnosed with polycystic ovary syndrome (PCOS) aged 22 her GP told her the symptoms could only be managed and to come back when she wanted to have a baby. Thirty years on, she says women are still being given the same advice.
PCOS is a hormonal disorder where ovaries produce large amounts of male sex hormones that interfere with the development and release of the eggs, which can affect periods and fertility.
Mrs Allan, 51, is from Leigh-on-Sea, Essex, and works as a nutritionist, says her PCOS symptoms included hair loss, facial hair, feeling low and gaining weight.
"When I have calls with women who are young and they are given the same advice I was given 30 years ago, [it] makes me feel so sad that we haven't moved forward," she says.
One in eight women in the UK are affected by PCOS, according to the charity Verity.
At the time of her diagnosis Mrs Allan was living in London and working in the children's book industry.
When she went to her GP about her condition she says she felt blamed for her symptoms because of her weight.
"There is nothing we can do - go on the pill and come back and see me when you want to have a baby," she says the doctor told her.
After that appointment, she says the GP surgery offered no further information.
"One of the symptoms of PCOS can be fertility, but not every woman has that and not every person with PCOS wants to have a baby," she says.
The now mother-of-two said she was not thinking about having children at 22.
"Once their diagnosis is confirmed, [patients with PCOS] are generally offered the contraceptive pill.
"It's not really getting to the root cause of your condition.
"I don't think it should be a bog standard - one-size-fits-all approach," she says.
At the time the internet was still in its infancy, so Mrs Allan said she turned to dieting groups as a way to manage her symptoms on the understanding that they were due to her weight.
Verity found only 3% of PCOS patients felt informed by their healthcare provider and 28% felt like their symptoms were not taken seriously.
"The lack of public awareness delays diagnosis and leaves many patients struggling alone with symptoms they don't understand," the report stated.
 Supplied
Supplied
Charlotte Notley was diagnosed with PCOS in 2021 and says she has turned to social media for help with her symptoms
Charlotte Notley, 34, from Norwich, was diagnosed with insulin resistance PCOS in 2021 and says the GP offered her the pill and would only refer her to a gynaecologist if she wanted to have a baby.
She says living with PCOS has made her feel like she is not normal, adding: "I don't know what it is like to wake up and not have a horrendous migraine or have pain in my ovaries or my uterus."
Mrs Notley says the lack of information led her to turn to social media and Chat GPT to find out more about her symptoms.
"Social media, as scary as it is, has been my doctor for the past 18 months.
"I shouldn't have to use social media and use advice of others and what they've tried and tested in order to manage a condition that isn't curable.
"I should be able to go to my GP and ask what are the best things I can do," she says.
In 2024, Mrs Notley says she stopped seeking help from the GP over the condition.
"I just wasn't getting anywhere and I was tired of being told that I was too fat all the time," she says.
 Supplied
Supplied
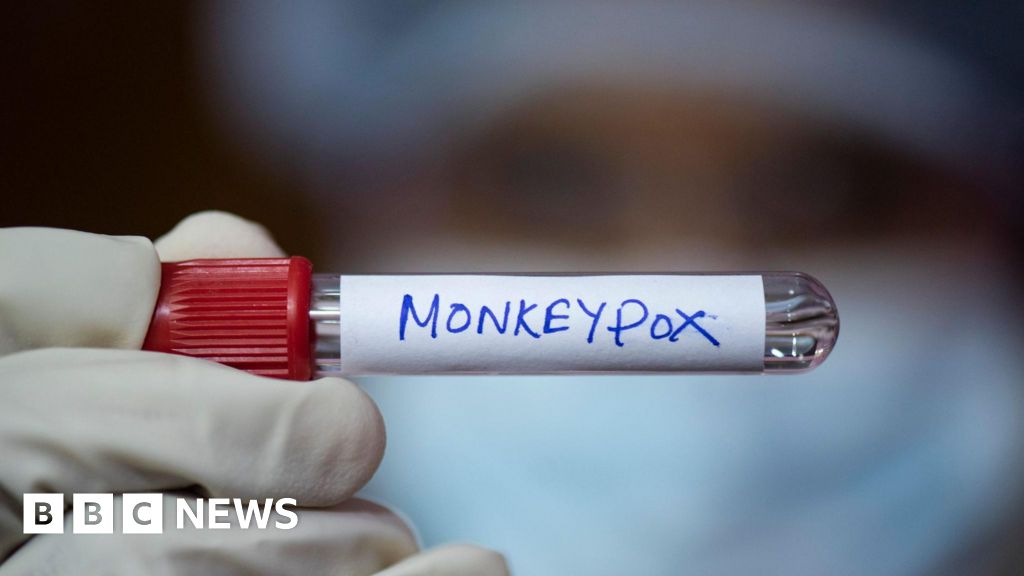
Rahat Khan, 50, is a consultant obstetrician and gynaecologist and says PCOS is a complex issue
Rahat Khan, 50, a NHS consultant obstetrician and gynaecologist at Phoenix Hospital Chelmsford, says: "PCOS is a condition, it is not a disease, it can affect periods and fertility.
"It is a difficult condition to diagnose and there is no cure for it.
"It is not appropriate to blame anyone for being overweight or for having PCOS because that can affect their mental wellbeing in an adverse manner.
"It is important to touch base with your GP or gynaecologist rather than self-treating yourself or trying to find solutions because that might not be very helpful."
Chand Kaur, 27, the founder of PCOS Relief, said the charity supports 2,500 people worldwide and that although she felt there had been research into the condition internationally, there has not been enough to make "a huge breakthrough".
"A lot of research now has come from Australia, so Australia is now leading the way in terms of PCOS," she says.
"I think medicine has advanced but in terms of the diagnosis and the terminology [around PCOS] - I think that it is very much the same," she says.
Mrs Kaur says a PCOS diagnosis often comes with the stigma of being infertile.
She adds, however, that once pregnant 65% of women with PCOS carry to full term, though they may face higher risks of complications such as gestational diabetes or preeclampsia.
Sue Mann, the national clinical director for women's health at NHS England, said: "We are acutely aware that too many women with conditions like polycystic ovary syndrome have struggled to get the help they need.
"That's why we're taking action to improve services and experiences for women, including rolling out women's health hubs across the country.
"With so much content circulating online, it is so important that women get clear, personalised advice from trusted NHS professionals."
A spokesperson from the Department of Health and Social Care said: "Women with polycystic ovary syndrome have been failed for too long.
"We're updating guidance for clinicians, improving training, tackling medical misogyny and have renewed our Women's Health Strategy to make sure every woman gets the care they deserve."

 German (DE)
German (DE)  English (US)
English (US)  Spanish (ES)
Spanish (ES)  French (FR)
French (FR)  Hindi (IN)
Hindi (IN)  Italian (IT)
Italian (IT)  Russian (RU)
Russian (RU)  3 weeks ago
3 weeks ago























Comments