James GallagherHealth and science correspondent
 Getty Images
Getty Images
Side effects of different antidepressants have been ranked for the first time, revealing huge differences between drugs.
Academics looked at the impact medications had on patients in the first eight weeks after starting treatment, with some causing patients to gain up to 2kg in weight or vary heart rate by as much as 21 beats every minute.
Around eight million people in the UK take antidepressants.
Researchers warned the gulf in side effects could affect people's health and whether they could stick to their prescription.
They said nobody reading this should stop their treatment, but have called for antidepressants to be closely matched to the needs of each person.
"There are big differences between [antidepressants] and this is important not just for individual patients, but large numbers of people are taking them, so even modest changes could have a big effect across the whole population," said researcher Prof Oliver Howes.
We've always known antidepressants affect physical health. The study by King's College London and the University of Oxford is the first to produce a ranking so the effects of medicines can be easily compared.
The team analysed 151 studies of 30 drugs commonly used in depression, involving more than 58,500 patients.
Not everybody develops side effects but, on average, the results published in the Lancet medical journal showed:
- An eight-week prescription of agomelatine was linked to a 2.4kg drop in weight compared with maprotiline, which led to nearly 2kg of weight gain
- A difference of 21 beats per minute between fluvoxamine, which slowed the heart, and nortriptyline, which sped it up
- An 11 mmHg difference in blood pressure between nortriptyline and doxepin
"Clearly no two antidepressants are built the same," said Dr Atheeshaan Arumuham, from King's College London.
Those differences can stack up in ways that become clinically important, including an increased risk of heart attack or stroke.
It means even people with the same diagnosis could be better suited to different antidepressants depending on their own preferences and other health conditions.
Dr Toby Pillinger told BBC Radio 4's Today programme: "The majority of the studies we looked at were relatively short. We're looking at eight weeks' duration and still within that duration we were seeing large changes in physical health parameters which we would argue have clinical relevance.
"The last thing I want is for this story to be scaring people," he added.
"I want to see this as empowering individuals to take the initiative and to engage in shared decision-making with their practitioner."
Which antidepressant is best for me?
In a hypothetical scenario, Sarah, 32, John, 44, and Jane, 56, have all received the same depression diagnosis and have been recommended antidepressants.
But they each want to avoid different side effects.
For Sarah, the priority is avoiding weight gain, while John already has high blood pressure and Jane has raised cholesterol.
Dr Pillinger, who worked through the examples for the BBC, says each would be recommended a different medicine.
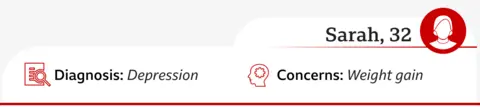
Dr Toby Pillinger says: Sarah should have an antidepressant that avoids weight gain, such as agomelatine, sertraline or venlafaxine rather than amitriptyline or mirtazapine which are more likely to increase weight.
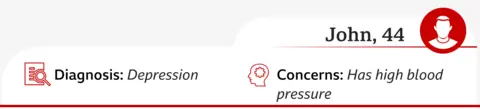
Dr Toby Pillinger says: John should avoid drugs such as venlafaxine, amitriptyline or nortriptyline which raise blood pressure, and would be better suited to citalopram, escitalopram and paroxetine.
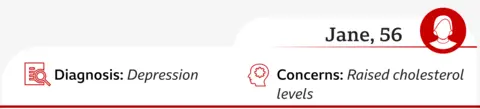
Dr Toby Pillinger says: For Jane, some antidepressants are linked to higher cholesterol, including venlafaxine, duloxetine and paroxetine, so she might steer clear of those. Citalopram or escitalopram are more neutral on cholesterol and could suit her better.
Push for 'generic, cheap medications'
It is too simplistic to say there are good and bad antidepressants, the researchers say. Even though amitriptyline increases weight, heart rate and blood pressure it also helps with pain and struggling to sleep.
Overall, the most prescribed class of antidepressants - SSRIs such as paroxetine, citalopram, escitalopram and sertraline - tended to have fewer physical side effects.
Fluoxetine - an SSRI that is also called Prozac - was linked to a drop in weight and higher blood pressure, in the study.
Prof Andrea Cipriani from the University of Oxford said it was "impossible" to say how many of the millions of people being prescribed antidepressants should be on a different drug.
However, he said there had been a push for "generic, cheap medications" that meant 85% of antidepressant prescriptions in the UK were for just three drugs: the SSRIs citalopram, sertraline and fluoxetine.
He said implementing the findings of this report would see "the 85% reduce dramatically" with "more people accessing better treatments".
The researchers are developing a free online tool to help doctors and patients choose the right drug.
However, that would still require a significant change in culture within the NHS.
The study also only analysed what happened eight weeks after starting treatment. Dr Pillinger said "complimentary data" meant they expected the short-term changes "will persist" but this still needs to be properly tested.
Dr Prasad Nishtala, from the University of Bath which was not involved in the study, said the findings were "novel and valuable".
He said: "In a real-world setting, where patients often receive antidepressants for months or years, the cumulative risks are likely to be higher, particularly among those with chronic depression."

 German (DE)
German (DE)  English (US)
English (US)  Spanish (ES)
Spanish (ES)  French (FR)
French (FR)  Hindi (IN)
Hindi (IN)  Italian (IT)
Italian (IT)  Russian (RU)
Russian (RU)  2 weeks ago
2 weeks ago























Comments