For Erica L and her husband, in-vitro fertilization was the “nuclear option”.
After two years of trying to conceive, Erica and her husband had no idea why they could not have a baby. Doctors said only that they had “unexplained infertility”, a non-diagnosis of a diagnosis that is given to an estimated 15% of people trying to conceive. Erica was not ideologically opposed to trying IVF, but felt daunted by the price and unpredictability.
Then Erica stumbled across a clinic that specialized in “restorative reproductive medicine”, or RRM. The clinic did bloodwork on Erica and her husband and urged them to eat well-balanced foods and take supplements, as well as prioritize exercise and sleep. Erica also started tracking her temperature and menstrual cycle in intense detail.
“We wanted to do everything that we could to try to have a baby as naturally as possible,” said Erica, who asked that her full last name not be published. “There’s a lot of invasive things that I just wasn’t comfortable with.”
Restorative reproductive medicine is a decades-old name for a constellation of therapies that are meant to revive the “natural” fertility of people trying to conceive. Often, RRM entails prescriptions for hormones, supplements and lifestyle changes - such as adopting a better diet - as well as closely analyzing one’s menstrual cycle. Its practitioners also sometimes use aggressive surgeries to root out endometriosis, a common and chronic condition that occurs when tissue that is similar to uterine tissue grows outside of the uterus. And, critically, RRM practitioners avoid the use of assisted reproductive technology such as IVF.
Top Republicans, rightwing organizations and even White House officials have recently begun to rally behind RRM, seizing on its promise to enhance fertility without resorting to IVF. Many anti-abortion conservatives revile IVF because it can create unused embryos – a practice they see as unethical, if not murderous, as they believe life begins at conception.
Yet IVF remains staggeringly popular, to the point that Donald Trump pledged to make it free in the wake of a 2024 Alabama supreme court decision that imperiled the procedure. Now, conservatives are trying to pare back that commitment – and some fertility doctors, including ones who offer RRM, worry that the right is co-opting RRM as a Trojan horse in order to sell a fertility agenda to voters while undermining IVF.
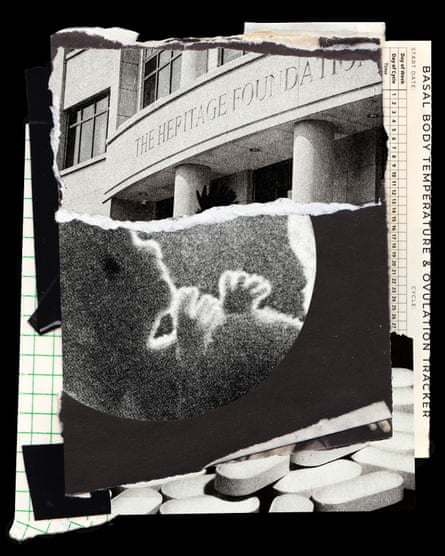
Backed by several high-profile anti-abortion groups, Republicans in Congress have repeatedly introduced legislation to bolster government-funded research and education on RRM. In March, the Heritage Foundation – the influential thinktank behind the notorious Project 2025 – released a 63-page report that endorsed RRM and slammed IVF.
Then, in July, the Department of Health and Human Services posted a notice soliciting applications for a $1.5m grant to fund an “infertility training center” that would expand access to resources for “holistic infertility treatments” rather than assisted reproductive technology. In August, the Washington Post reported that the Trump administration is backing away from the president’s campaign promises about IVF, although a White House spokesperson rebutted that claim.

Dr Kaylen Silverberg is a reproductive endocrinologist who has advised administration officials, including Trump’s chief of staff Susie Wiles, about IVF. During his discussions with officials, Silverberg said he was asked about RRM.
“I’ve been doing this for 31 years, and I’d never even heard the term,” said Silverberg, who is also advisory board chair of the advocacy group Americans for IVF. “So I started doing research about it. I realized that restorative reproductive medicine is just a pseudonym for a basic infertility evaluation.”
Silverberg’s view is shared by many mainstream fertility doctors and organizations, who say that the difference between their work and RRM is less scientific than ideological. In their view, RRM is a rebranded version of everyday fertility medicine, minus IVF.
RRM, with its focus on optimizing the body’s “natural” rhythms, is tapping into a growing interest in holistic health and wellness – one that is being increasingly politicized and expertly leveraged by the “Make America Healthy Again” (Maha) movement.
But support for RRM alone, Silverberg said, cannot fulfill Trump’s campaign promises. “The problem is going to be if – and this is a big if – anybody tries to limit expansion of fertility access and care and coverage to restorative reproductive medicine.”
‘There is another option’
RRM is not a monolith. Some of its leading organizations and adherents take no position on IVF and reject the idea that RRM is ideologically driven or a new name for old medicine. Instead, they are drawn to RRM’s stance that infertility is not itself a disease but a symptom of something else that has gone wrong.
Established in 2000, the International Institute for Restorative Reproductive Medicine (IIRRM), the preeminent group championing RRM, maintains a registry of RRM clinicians and collects data about its techniques’ efficacy.
Dr Monica Minjeur, who was trained in family medicine and serves as the US director of communications and development for the International Institute for Restorative Reproductive Medicine, said RRM is “not an anti-IVF movement”. As far as Minjeur knows, no one in Congress has approached the institute to discuss RRM.
“We will never say: ‘IVF should go away.’ We just mostly want people to realize: ‘Hey, there is another option,’ because so many couples are told IVF is your only option,” said Minjeur, who added that she is a Democrat.

Some RRM advocates and groups do oppose IVF and have long aligned themselves with conservative causes such as the anti-abortion movement. One of the most well-known RRM techniques is NaPro Technology, which usually involves such tactics as cervical mucus tracking and has been pioneered by the anti-abortion Saint Paul VI Institute since the 1980s, when the Vatican condemned IVF. The institute’s website presents NaPro Technology as an alternative to IVF, which it calls “a highly abortive technology that often forces women to make abortion-related decisions”.
In June, a new thinktank, the Maha Institute, held a roundtable discussion about women’s health and fertility. In her introduction to the discussion, Maureen Ferguson, a commissioner for the US Commission on International Religious Freedom with longstanding ties to the anti-abortion movement, sang RRM’s praises.
“Traditional women’s health and fertility care has relied heavily on big pharma bandaids and workarounds that circumvent a women’s reproductive system,” Ferguson said. “Women of all political stripes appreciate healthcare that works in harmony with their body and restores health.”
IIRRM wants to harness Maha advocates’ enthusiasm but is wary of being equated with the movement, according to Minjeur and Dr Tracey Parnell, the institute’s global director of communications and development. They described RRM and Maha as two sides of a Venn diagram.
“We want to bring increased health to women and men and families,” Minjeur said of Maha. “Beyond that, there are definitely a fair amount of differences.”
Parnell added: “We really truly are open to quite broad collaboration without being co-opted.”
The rise of wellness culture
The Make America Healthy Again movement is perhaps the best illustration of a broader push within American conservatism to incorporate the historically leftwing language of holistic health and “natural” treatments – in short, “wellness” – to advocate for traditionally rightwing aims, such as convincing women to have big families.
This push started to gain steam in the years after the Covid pandemic, as trust in mainstream medicine started to falter: a survey of nearly half a million US adults found that trust in physicians and hospitals declined from roughly 72% to just 40% between April 2020 – the month after the pandemic broke out – and January 2024. As trust eroded, the wellness industry exploded. Between 2019 and 2023, it grew from $5.3tn to $6.32tn, according to the Global Wellness Institute, which defines wellness as the ongoing and individual pursuit of “optimal holistic health and wellbeing”.
“Wellness” can encapsulate a wide range of activities, from undeniably healthy behaviors (such as exercising and eating nutritious foods) to practices that may be dangerous (such as drinking raw milk). These activities are yoked together by a deceptively simple ethos, according to Amy Larocca, author of the book How to Be Well: Navigating Our Self-Care Epidemic, One Dubious Cure at a Time.
“In wellness, things that are natural are superior to things that are not,” Larocca explained.
Wellness’s sales pitch can be particularly appealing to Americans, given the astronomical costs of traditional healthcare in the US. A single IVF cycle can run tens of thousands of dollars and most states do not require insurers to cover it. By contrast, countries such as Denmark and Sweden cover vast swathes of fertility treatments, including IVF.
RRM treatments tend to cost far less than IVF, and may soon get even cheaper. In June, Arkansas’s Republican-dominated state legislature became the first in the country to pass a law requiring state insurance to cover RRM therapies.
But critics say there is little quality evidence that RRM is more effective at helping people have babies than mainstream fertility medicine. The American Society for Reproductive Medicine, the American College of Obstetricians and Gynecologists, the Society for Maternal-Fetal Medicine and the Society of Gynecologic Surgeons are worried that other states may follow Arkansas’s lead; last week, the medical organizations sent a letter to urging the National Governors Association to reject pro-RRM legislation.
Women’s health and infertility are especially ripe breeding groups for wellness because mainstream medicine routinely fails to take either seriously. Between 2013 and 2023, just 8.8% of research funded by the National Institutes of Health focused on women’s health. Women are also more likely to have their medical concerns dismissed. When women and people of color show up at emergency rooms with signs of chest pain, they usually wait longer; women are also less likely to be admitted.
‘Many sobbing women’
A year after Erica started working with the restorative reproductive medicine clinic, the clinic told her: “We’re really concerned that you’re not pregnant yet. You should be pregnant.”
The RRM specialists suggested that Erica might have endometriosis, which affects about one in 10 women and girls worldwide and is believed to be a leading cause of infertility.
It is also profoundly understudied. In 2023, a mere 0.06% of the NIH’s $47bn budget was earmarked for endometriosis research. Because many doctors dismiss the symptoms of endometriosis or lack the expertise to recognize it, it generally takes between five and 11 years to get a diagnosis.
Erica went ahead with a surgery to diagnose and remove endometriosis tissue. RRM practitioners have suggested that the condition can be treated by a “one-and-done surgery” – as one RRM surgeon put it in the Heritage Foundation report – that aggressively excises endometriosis tissue.
A month later, Erica got pregnant. Erica estimated that she and her husband spent, in total, about $2,500 on RRM.
“We definitely wouldn’t have our daughter without them,” she said of RRM specialists.

Many of RRM’s prescriptions are common sense: if you are trying to get pregnant, it can be helpful to take a holistic view of your health and know as much about your menstrual cycle as possible. But mainstream reproductive endocrinologists are skeptical of RRM’s position that infertility itself is not a disease, which runs counter to the World Health Organization’s definition of infertility. They also suspect that RRM may over-rely on surgery to treat endometriosis. One recent review of infertility treatments published in the New England Journal of Medicine found that while surgery can help mild cases of endometriosis, doctors should use IVF when it is severe. When treated with IVF, almost 40% of women under 35 who have endometriosis get pregnant within a single cycle, the review found.
“We do a lot of surgery and other treatment options that can optimize a woman’s fertility. But in the end, there are many diagnoses that cannot be solved with those elements alone and need a very effective tool like IVF,” said Dr Rachel Weinerman, a reproductive endocrinologist and associate professor at Case Western Reserve University’s school of medicine. “You need to have a whole toolbox available to decide what is the right tool for that specific patient.”
Dr Eve Feinberg, a reproductive endocrinologist at Northwestern University’s Feinberg school of medicine, first heard of RRM when she started treating patients who had tried it. If patients stick with RRM and defer the use of assisted reproductive technology for too long, Feinberg warned, some may become so old that they lose their chance to have biological children.
“I’ve had many sobbing women in my office who really missed out on their fertility window by trying endless numbers of years of this method, who weren’t given the truth and weren’t given a chance to explore other methods because they were misled and they were told that this would work for them,” she said. “I counsel my patients that IVF has limitations. It doesn’t work for every patient. I didn’t feel like these women were adequately counseled in that way.”
In an extensive memo it shared with the Guardian, IIRRM rejected many of the critiques of RRM as unfounded, including the idea that it over-relies on surgery. Physicians who provide IVF too often default to it, the institute contended, adding that it would welcome more research comparing RRM to conventional medicine.
As someone who eats a mostly plant-based diet, runs religiously and avoids makeup, Feinberg considers herself to be more “natural” than most. She understands the appeal of the wellness-style language that surrounds RRM.
“It’s being marketed as being holistic. It’s being marketed as being natural and ethical,” Feinberg said. But, she continued: “I think RRM plays into this fallacy that we can understand everything and we can fix everything. And it’s just not true.”

 German (DE)
German (DE)  English (US)
English (US)  Spanish (ES)
Spanish (ES)  French (FR)
French (FR)  Hindi (IN)
Hindi (IN)  Italian (IT)
Italian (IT)  Russian (RU)
Russian (RU)  3 weeks ago
3 weeks ago
























Comments